Is my semen infected? Everything you need to know about leukocytospermia
What is leukocytospermia?
Leukocytes are white blood cells, which protect the body against infectious diseases and foreign invaders. An increase in leukocytes in the body can be a sign of infection or inflammation. These leukocytes are commonly found in semen samples. Leukocytospermia, or pyospermia, is defined as the presence of more than 1 million white blood cells in 1 mL of ejaculate.
What causes leukocytospermia?
Leukocytospermia can be a result of infection or inflammation anywhere along the genitourinary tract, particularly the prostate gland, seminal vesicles, testicles, and bulbourethral glands, which produce the fluid in semen. The presence of these leukocytes is not completely understood, but they can be seen in the following conditions: urinary tract infection, sexually transmitted infections, autoimmune conditions, urethral strictures, varicoceles (dilated veins around the testicle), systemic illness, and use of tobacco, marijuana, or alcohol. Some studies have shown that long periods of abstinence from ejaculation can increase the number of leukocytes in the semen. Leukocytospermia is often idiopathic, which means that we don’t know where these leukocytes are coming from.
What are the symptoms of leukocytospermia?
Often times, patients diagnosed with leukocytospermia will have no symptoms. However, sometimes they will show symptoms of an infection in the bladder, prostate, epididymis, or testicle, consistent with cystitis, prostatitis, epididymitis, or orchitis, respectively. These symptoms include urinary frequency, painful urination, pelvic pain, testicular pain, and pain with ejaculation.
What is the impact of leukocytospermia?
The presence of leukocytes in the semen can affect overall sperm health. Leukocytes can weaken the sperm and damage its genetic material. Leukocytes can release substances called reactive oxygen species, which can negatively impact sperm. Leukocytes can increase DNA damage of sperm (DNA fragmentation). Leukocytes can cause sperm clumping and affect the motility of sperm, which can make it harder to become pregnant. Some studies show an increased pregnancy rate through natural conception in men who have been treated adequately for leukocytospermia. There is no evidence that leukocytospermia has any negative impact on in vitro fertilization (IVF) outcomes, including rates of fertilization, embryo development, quality of embryos, and pregnancy following embryo transfer.
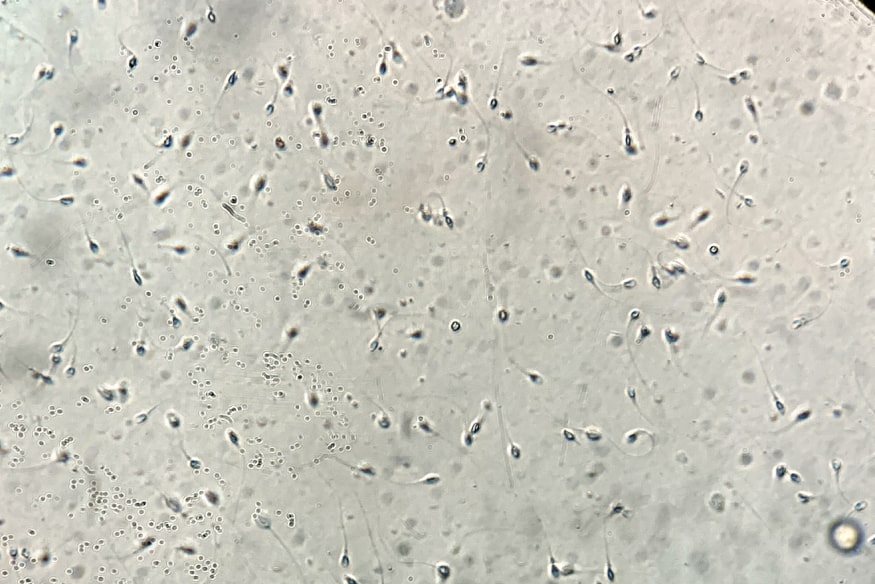
How is leukocytospermia diagnosed?
Leukocytospermia is diagnosed by an andrologist during a semen analysis. The andrologist examines the semen under a microscope and counts the number of white blood cells and calculates an estimate of the number of white blood cells per mL of semen. A thorough history and physical exam by a male infertility specialist can help determine if there is an obvious source of infection. A urine culture or semen culture can be done to see if there is bacteria that grows in the urine or semen. The American Urological Association (AUA) and American Society of Reproductive Medicine (ASRM) recommend quantifying the number of leukocytes in the semen in patients with unexplained male infertility or for evaluation of assisted reproductive options.
How is leukocytospermia treated?
There is no consensus regarding the treatment of leukocytospermia. AUA and ASRM do not have any treatment recommendations, while the Canadian Urological Association (CUA) recommends that therapy be considered in the setting of infertility and the European Association of Urology (EAU) states that antibiotics may improve sperm quality, but that there is no definitive evidence that it increases the probability of conception. Ultimately, treatment should be determined on a case by case basis. In patients who prefer to get pregnant through natural conception or intrauterine insemination (IUI) and have leukocytospermia along with low sperm motility, it may be more appropriate for treatment. Treatment options include long courses of antibiotics (usually 4-6 weeks), anti-inflammatory medication (i.e. ibuprofen), steroids, anti-histamines, and antioxidants, though the data on these treatment regimens in limited. If urine or semen cultures are positive, antibiotic therapy can be targeted. However, most cases of leukocytospermia result in negative cultures. Thus, empiric antibiotics can be used that target the typical organisms that cause prostatitis. These antibiotics include tetracyclines (i.e doxycycline), sulfonamides (i.e. Bactrim), quinolones (i.e. ciprofloxacin), macrolides, and penicillins. Some studies have shown frequent ejaculation (at least every three days) can help reduce the number of leukocytes. Cessation of tobacco, marijuana, and alcohol may also reduce the number of leukocytes in the semen. Some studies have shown that treatment of leukocytospermia may lead to higher pregnancy rates, though data is limited and there is a need for more better quality research.
Will leukocytospermia prevent me from having children?
Ultimately, this is probably the most important question for our patients. If our patients are struggling to conceive, it is unlikely that leukocytospermia is the only underlying cause. These leukocytes may make it a little more difficult to get pregnant, but certainly not impossible. Many of our patients with leukocytospermia are still able to get pregnant through a variety of methods: natural conception, IUI, and IVF. Since the presence of these leukocytes is not well understood, some urologists choose to never treat them while others treat them in every instance. At Reproduce Medicine Associates of New Jersey, we take a different approach. Our urologists treat them in some instances where the benefits may outweigh the risks and only if our patients are comfortable with the treatment plan.
IVIRMA ) Innovation
Source: https://www.ivi-rmainnovation.com/everything-you-need-to-know-about-leukocytospermia/


Leave A Comment